Highlight
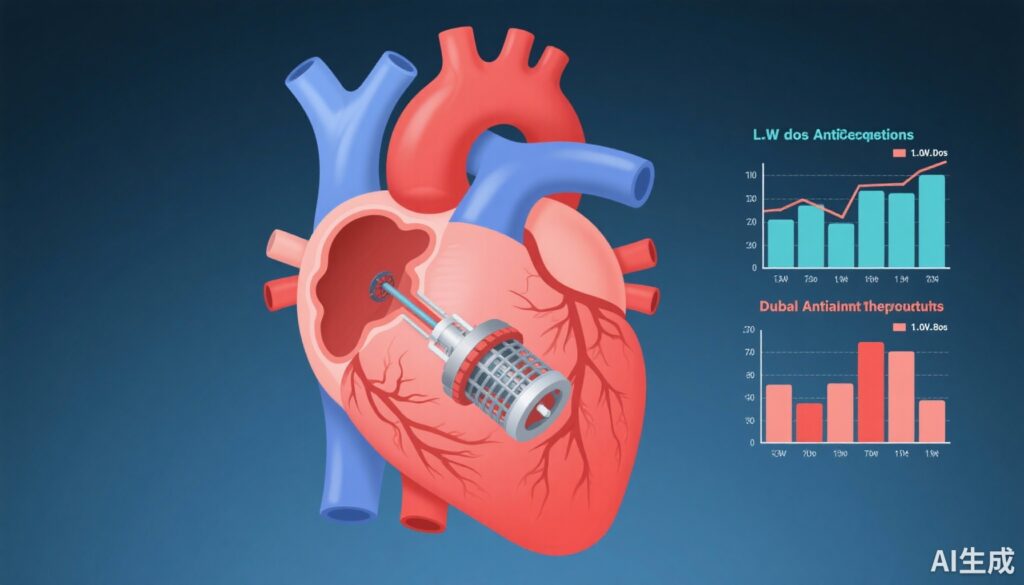
- The ADALA trial evaluated 3-month post-procedural strategies after left atrial appendage occlusion (LAAO) using low-dose apixaban versus dual antiplatelet therapy (DAPT).
- Low-dose apixaban significantly reduced the composite primary endpoint of major bleeding and thromboembolic events compared to DAPT (4.5% vs 21.7%).
- Device-related thrombosis (DRT) was absent in the low-dose apixaban group versus 8.7% incidence with DAPT.
- No strokes or systemic embolism events were observed in either group during follow-up.
Study Background and Disease Burden
Atrial fibrillation (AF) substantially increases stroke risk due to thrombus formation primarily in the left atrial appendage (LAA). LAA occlusion (LAAO) devices provide an alternative to oral anticoagulation (OAC) for stroke prevention, particularly in patients at high bleeding risk or with contraindications to long-term OAC. Post-LAAO antithrombotic management remains controversial, with international practice varying between short-term anticoagulation and dual antiplatelet therapy (DAPT). DAPT has been widely used but may carry higher thrombotic risk, including device-related thrombosis (DRT), and anticoagulation carries bleeding concerns. Thus, determining the optimal post-LAAO regimen balancing efficacy and safety is an unmet clinical need.
Study Design
The ADALA trial was a prospective, multicenter, open-label randomized clinical trial conducted at three European centers between June 2019 and August 2022. Successful LAAO patients were randomized 1:1 to receive either low-dose apixaban (2.5 mg twice daily) or DAPT (aspirin 100 mg plus clopidogrel 75 mg daily) for the first 3 months post-procedure. The trial prematurely terminated after recruiting 90 patients (60% of planned enrollment) due to COVID-19-related recruitment challenges. The primary composite end point included major bleeding (safety) and thromboembolic events (stroke, systemic embolism, and DRT; efficacy) evaluated over the first 3 months post-LAAO. Secondary endpoints encompassed individual components of the primary outcome and all bleeding events.
Key Findings
The analysis included 90 patients (mean age 76.6 years, 66.7% male) with mean CHADS-VASc score 4.0 and a high prevalence of prior major bleeding (58.8%), dominantly gastrointestinal (66.7%) and intracranial (17.8%). Forty-four patients received low-dose apixaban, while 46 received DAPT.
At 3 months, the low-dose apixaban group showed a significantly lower primary endpoint rate (4.5%) compared to DAPT (21.7%), with a hazard ratio of 0.19 (95% CI, 0.04–0.88; P = .02). This difference was mainly driven by fewer device-related thrombotic events: 0% in the apixaban group versus 8.7% with DAPT (P = .04). Major bleeding events tended to be less frequent with apixaban (4.6% vs 13.0%; P = .17), although this did not reach statistical significance. Notably, no strokes or systemic embolism events occurred in either group.
The composite data suggest that low-dose apixaban post-LAAO may provide improved safety and thromboembolic protection compared to standard DAPT in a high-risk population. The absence of stroke despite reduced anticoagulation intensity suggests adequate efficacy of low-dose DOAC in preventing clinically relevant thromboembolic complications.
Expert Commentary
The ADALA trial adds important prospective randomized evidence supporting the use of low-dose direct oral anticoagulants (DOACs), specifically apixaban, following LAAO—a strategy not extensively studied previously. The findings challenge the traditional widespread use of DAPT in this setting, highlighting that even a reduced anticoagulant dose can reduce device-related thrombosis without increasing major bleeding risk. This trial’s strengths include its randomized design and focus on a high bleeding risk cohort.
Limitations include the relatively small sample size and early termination, which may limit generalizability and power to detect differences in less frequent endpoints such as stroke or systemic embolism. Moreover, the open-label nature could introduce bias. Nonetheless, the significant reduction in DRT with low-dose apixaban is biologically plausible given the anticoagulant’s mechanism targeting thrombin generation. Future larger trials can validate these findings and refine antithrombotic protocols post-LAAO.
Current European guidelines acknowledge the lack of consensus on post-LAAO therapy and recommend individualized strategies considering bleeding risk, patient comorbidity, and device characteristics. This trial provides preliminary evidence favoring low-dose anticoagulation as a safe and effective alternative to dual antiplatelet therapy in the immediate post-procedural period.
Conclusion
In patients undergoing successful left atrial appendage occlusion, short-term low-dose apixaban appears superior to dual antiplatelet therapy in reducing the composite risk of major bleeding and thromboembolic events, principally driven by lower device-related thrombosis. No stroke or systemic embolism events were observed in either group within the 3-month follow-up. These findings suggest low-dose direct oral anticoagulation may better balance efficacy and safety compared with DAPT in this high-risk population. However, further large-scale randomized studies are required to confirm these results and optimize post-LAAO management guidelines.
References
1. Freixa X, Cruz-González I, Cepas-Guillén P, et al. Low-Dose Direct Oral Anticoagulation vs Dual Antiplatelet Therapy After Left Atrial Appendage Occlusion: The ADALA Randomized Clinical Trial. JAMA Cardiol. 2024;9(10):922-926. doi:10.1001/jamacardio.2024.2335.
2. Reddy VY, Doshi SK, Kar S, et al. 5-Year Outcomes After Left Atrial Appendage Closure: The PREVAIL and PROTECT AF Trials. J Am Coll Cardiol. 2017;70(24):2964-2975.
3. January CT et al. 2019 AHA/ACC/HRS Focused Update on Atrial Fibrillation. Circulation. 2019;140:e125–e151.