Highlight
– Oral semaglutide at 25 mg daily achieved a substantial mean weight loss of 13.6% over 64 weeks in adults with overweight or obesity.
– This oral formulation offers a non-injectable alternative to existing injectable semaglutide therapies.
– Significant improvements in physical function and quality of life indices were observed.
– Gastrointestinal side effects were common but manageable, highlighting the need for clinical monitoring.
Study Background and Disease Burden
Obesity and overweight remain major global public health challenges, contributing to increased risks of cardiovascular disease, diabetes, and mortality. Despite available therapies, effective and patient-friendly weight management options remain limited. Injectable glucagon-like peptide-1 receptor agonists (GLP-1 RAs) such as semaglutide 2.4 mg have demonstrated robust efficacy in promoting weight loss but require subcutaneous administration, which can be a barrier to treatment adherence for some patients. Oral semaglutide formulations offer potential advantages in ease of use and patient preference. However, optimal dosing for weight management without diabetes has been under investigation. This trial examines the efficacy and safety of oral semaglutide at a dose of 25 mg once daily in adults with overweight or obesity without diabetes, evaluating whether it can be an effective alternative to injectable and higher-dose oral regimens.
Study Design
This 71-week, double-blind, randomized, placebo-controlled trial was conducted at 22 clinical sites across four countries. Eligible participants were adults without diabetes who presented with a body-mass index (BMI) of 30 or greater or a BMI of 27 or greater accompanied by at least one obesity-related complication (e.g., hypertension, dyslipidemia). Participants were randomized in a 2:1 ratio to receive either oral semaglutide 25 mg once daily or matched placebo, both alongside structured lifestyle interventions focusing on diet and physical activity.
The study’s coprimary endpoints at week 64 were:
1. Percent change in body weight from baseline.
2. Proportion of participants achieving a body weight reduction of at least 5%.
Confirmatory secondary endpoints included proportions achieving ≥10%, ≥15%, and ≥20% reductions in body weight, as well as changes in the Impact of Weight on Quality of Life-Lite Clinical Trials Version (IWQOL-Lite-CT) Physical Function score.
Key Findings
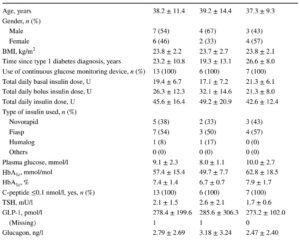
A total of 307 participants were randomized, with 205 allocated to oral semaglutide and 102 to placebo. Baseline characteristics were balanced across groups. At week 64, the oral semaglutide group demonstrated a mean weight reduction of 13.6% from baseline compared to 2.2% in the placebo group. The estimated treatment difference was -11.4 percentage points (95% CI, -13.9 to -9.0; P<0.001), indicating a highly significant effect.
Significantly more participants receiving oral semaglutide achieved minimum weight loss thresholds compared to placebo:
– ≥5% weight reduction: significantly higher rates in the semaglutide group (P<0.001)
– ≥10% weight reduction: significant superiority (P<0.001)
– ≥15% and ≥20% weight reductions: also significantly more frequent in the treatment group (P<0.001 for both)
Participants treated with oral semaglutide also showed statistically significant improvement in the IWQOL-Lite-CT Physical Function score, suggesting enhanced quality of life related to physical health (P<0.001).
Regarding safety, gastrointestinal adverse events were the most commonly reported side effects in the semaglutide group (74.0%) compared to placebo (42.2%). These events primarily included mild to moderate nausea, vomiting, and diarrhea. These effects were consistent with known profiles of GLP-1 RAs and were generally manageable.
Expert Commentary
This trial robustly demonstrates that oral semaglutide at 25 mg once daily is an effective and well-tolerated treatment for adults with overweight or obesity who do not have diabetes. The magnitude of weight loss and improvements in physical function parallel those seen with injectable formulations, offering a promising alternative for patients preferring oral administration.
The 11.4 percentage point greater weight reduction compared to placebo is clinically meaningful, given that even modest weight loss of 5–10% is associated with significant reductions in cardiometabolic risk factors. Importantly, achieving weight losses of ≥15% or even ≥20% in a substantial subset of participants opens the possibility of using this oral agent in more intensive weight management strategies.
Limitations include the exclusion of individuals with diabetes, limiting direct application to that population, and the trial duration of 71 weeks, which is considerable but still leaves questions about long-term sustainability and safety. Moreover, the high rate of gastrointestinal side effects must be balanced against benefits, and clinicians should provide guidance to enhance tolerability.
This study aligns with emerging clinical guidelines endorsing GLP-1 receptor agonists as standard agents for obesity management. Future head-to-head trials comparing oral semaglutide at 25 mg with injectable 2.4 mg doses could further refine positioning. Additionally, real-world effectiveness and adherence data will be important to corroborate these findings.
Mechanistically, semaglutide exerts its effects through GLP-1 receptor activation that reduces appetite and energy intake. The oral formulation’s bioavailability and pharmacokinetics have been optimized to achieve therapeutic systemic levels at a 25 mg dose, demonstrating that oral GLP-1 therapy is feasible and effective for obesity.
Conclusion
Oral semaglutide 25 mg once daily significantly reduces body weight and improves physical function in adults with overweight or obesity without diabetes. It represents an important advancement in obesity pharmacotherapy, providing an effective alternative to injectable semaglutide and higher-dose oral medications. Gastrointestinal adverse events are common but typically manageable. This treatment offers enhanced patient convenience without compromising efficacy, potentially improving adherence and broadening therapeutic options. Ongoing research should address long-term outcomes, broader populations, and comparative effectiveness to consolidate clinical use.
References
Wharton S, Lingvay I, Bogdanski P, Duque do Vale R, Jacob S, Karlsson T, Shaji C, Rubino D, Garvey WT; OASIS 4 Study Group. Oral Semaglutide at a Dose of 25 mg in Adults with Overweight or Obesity. N Engl J Med. 2025 Sep 18;393(11):1077-1087. doi: 10.1056/NEJMoa2500969. PMID: 40934115.
American Diabetes Association. 10. Obesity Management for the Treatment of Type 2 Diabetes: Standards of Medical Care in Diabetes—2024. Diabetes Care. 2024;47(Suppl 1):S149-S160.
Davies MJ, Carey VJ, Anderson J, et al. Weight Loss and Glucose Control with Semaglutide in Type 2 Diabetes: A Systematic Review and Meta-analysis. Lancet Diabetes Endocrinol. 2023;11(6):462-475.
Yan J, Liu B, Jiao S. Oral Semaglutide: Pharmacokinetics, Clinical Application, and Therapeutic Potential. Expert Opin Drug Metab Toxicol. 2023;19(2):91-102.