Study Background and Disease Burden
Overweight and obesity represent pervasive public health challenges worldwide, contributing significantly to metabolic disorders, cardiovascular disease, and diminished quality of life. Nutritional interventions are central to managing weight, with interest growing in time-restricted eating (TRE) as a potential strategy. TRE limits daily food intake to a specified window, potentially improving metabolic health due to alignment with circadian rhythms. However, the impact of TRE, particularly the timing of the eating window, on measures beyond weight such as sleep quality, mood states, and overall quality of life, remains inadequately explored. Understanding these effects is critical, as disruptions in sleep, mood disorders, and impaired life quality are common comorbidities among individuals with overweight or obesity.
Study Design
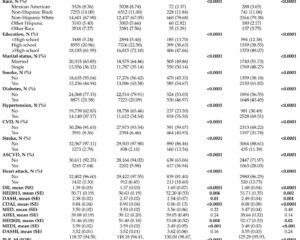
This investigation is a prespecified secondary analysis of a parallel-group randomized clinical trial conducted between April 2022 and March 2023 at sites in Granada and Pamplona, Spain. The study enrolled 197 men and women aged 30 to 60 years with overweight or obesity (mean BMI 32.8). Participants were randomized equally to one of four groups: usual care (UC) consisting of a Mediterranean diet education program maintaining habitual eating duration (≥12 hours), and three TRE intervention groups each following an 8-hour eating window combined with the UC educational program. TRE schedules included: early TRE (eating window starting before 10 am), late TRE (starting after 1 pm), and self-selected TRE (participants choosing their own 8-hour window). The intervention lasted 12 weeks.
Primary outcomes assessed were changes in objective sleep parameters, evaluated via accelerometry during the two weeks prior to and the final two weeks of the intervention phase. Secondary outcomes included self-reported mood metrics (depression, anxiety, stress) and quality of life, measured pre- and post-intervention using standardized questionnaires including the Beck Depression Inventory Fast Screen, State-Trait Anxiety Inventory, Perceived Stress Scale, and Rand 36-Item Short Form Health Survey.
Key Findings
Analysis of data from 197 participants (49.7% women; mean age 46.1 years) revealed no statistically significant differences between the TRE groups and usual care across sleep, mood, or quality of life parameters. Specifically, the difference in total sleep time between early TRE and UC was minimal (mean difference 0.2 hours; 95% CI, -0.2 to 0.6), indicating negligible effect from the eating window timing. Similarly, changes in mood scales showed overlapping confidence intervals with no significant improvement or worsening in depression scores (Beck Depression Inventory Fast Screen mean difference 0.2 points, 95% CI, -1.0 to 1.3), anxiety (State-Trait Anxiety Inventory mean difference -1.2, 95% CI, -6.4 to 4.1), or perceived stress (2.1 points; 95% CI, -1.8 to 5.9).
Quality of life assessed by general health scores also did not differ significantly between groups. The late TRE and self-selected TRE groups similarly showed no meaningful differences from the UC group or from each other in any evaluated outcome domain.
Importantly, the study found no adverse effects of TRE protocols on participants’ sleep architecture, mood states, or overall well-being during the 12-week period, suggesting safety of TRE interventions with respect to these outcomes.
Expert Commentary
Given the complex interplay between circadian rhythms, metabolism, sleep, and psychological health, some hypothesized benefits or detriments from TRE timing on sleep and mood. The null findings indicate that although TRE may facilitate weight management (as prior studies suggest), its timing—early morning versus late day versus self-selected—does not differentially impact these important psychosocial and sleep-related outcomes in the short term.
The study’s strength lies in the randomized controlled design, objective sleep assessment, and robust mood and quality of life measurement tools. However, limitations include the relatively short duration (12 weeks) which may not capture longer-term effects, and the secondary analysis scope primarily designed for weight and metabolic outcomes. Additionally, generalizability may be limited to middle-aged adults with overweight or obesity without severe mood disorders.
Future research should explore longer interventions, diverse populations, and incorporate mechanistic studies to elucidate how TRE interfaces with neurobehavioral health and circadian biology.
Conclusion
This randomized clinical trial’s secondary analysis demonstrates that incorporation of time-restricted eating schedules, whether early, late, or self-selected 8-hour windows combined with Mediterranean diet education, does not substantially alter sleep quality, mood, or quality of life compared with standard care in adults with overweight or obesity. These findings support the safety and tolerability of TRE in this population, underscoring its potential as a nutritional strategy for weight management without compromising multidimensional aspects of health. Clinicians may consider TRE as an adjunctive approach for patients seeking weight loss interventions, with reassurance regarding its neutral effects on sleep and psychosocial well-being.
References
Clavero-Jimeno A, Dote-Montero M, Migueles JH, et al. Time-Restricted Eating and Sleep, Mood, and Quality of Life in Adults With Overweight or Obesity: A Secondary Analysis of a Randomized Clinical Trial. JAMA Netw Open. 2025;8(6):e2517268. doi:10.1001/jamanetworkopen.2025.17268