Highlight
Recent research from the Framingham Heart Study generation 2 cohort demonstrates that a history of traumatic brain injury (TBI) is associated with significant reductions in hippocampal and cerebral gray matter volumes in older women, but not in men. This sex-specific brain volume loss was observed approximately 12 years after injury, underscoring the long-term neuroanatomical impact of TBI. These findings suggest that women may have greater vulnerability to TBI-related neurodegeneration, with potential implications for cognitive decline and dementia risk.
Clinical Background and Disease Burden
Traumatic brain injury (TBI) is a major public health concern affecting millions worldwide. It ranges from mild concussions to severe brain trauma and is a well-established risk factor for subsequent cognitive impairment and dementia. Despite advances in acute management, the chronic consequences of TBI remain a critical clinical challenge.
Sex differences in TBI outcomes have been increasingly recognized. Women and men may respond differently to brain injury due to biological and hormonal factors, yet few epidemiological or neuroimaging studies have rigorously explored these differences over the long term.
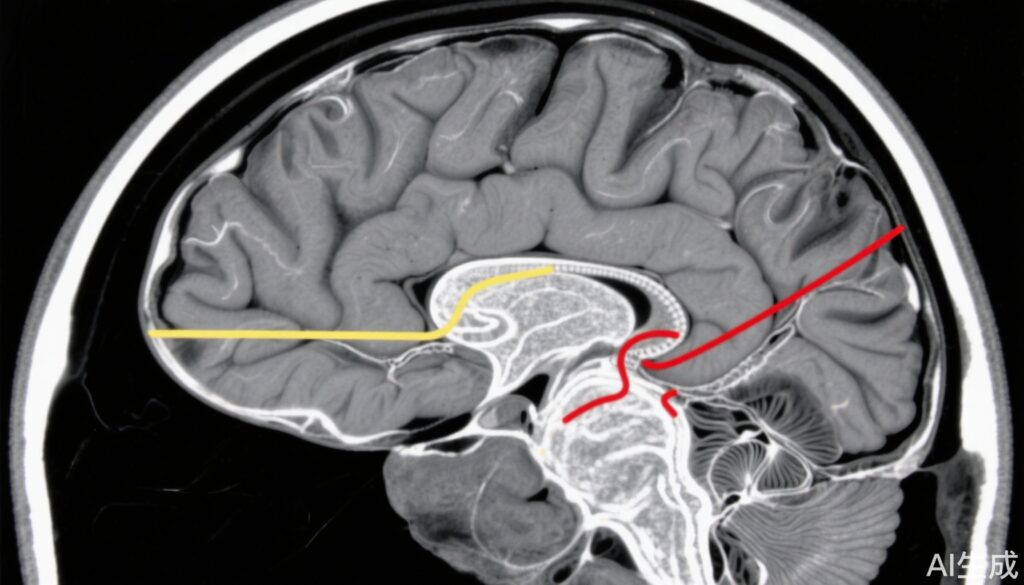
Brain atrophy detectable on magnetic resonance imaging (MRI), particularly in the hippocampus and frontal lobes, correlates with cognitive decline in aging and neurodegenerative diseases. Understanding how TBI contributes to structural brain changes later in life—and how these effects diverge by sex—can inform tailored interventions and prognosis.
Research Methodology
This investigation utilized data from the Framingham Heart Study generation 2 cohort, enrolling adults born between 1971 and 1975. The study identified 159 individuals with a history of TBI (141 classified as mild and 18 as moderate-to-severe) and matched each to four TBI-free controls (n=636) by birth year and sex. The mean age at MRI was 68 years, with an equal distribution of women and men.
All participants underwent brain MRI between 2005 and 2008, approximately 12 years after the reported TBI event on average. Volumetric MRI analyses quantified total and regional brain volumes, including hippocampal, frontal gray matter, and total cerebral gray matter volumes.
Statistical regression models adjusted for confounders such as total intracranial volume, education level, APOE ε4 genotype status, age at scan, and time since injury. Analyses were stratified by sex to investigate potential differences between women and men.
Key Findings
Overall, participants with a history of TBI had significantly smaller hippocampal volumes compared with controls without TBI (β= -0.15; P = .004). There was also a trend towards smaller frontal gray matter volume in the TBI group, although this did not reach statistical significance (β= -1.66; P = .056).
Stratified analyses revealed striking sex-specific effects. In women, TBI was strongly associated with smaller hippocampal volume (β= -0.25; P < .0001), reduced frontal gray matter volume (β= -2.67; P = .007), and decreased total cerebral gray matter volume (β= -5.20; P = .030). Conversely, men with TBI did not show significant differences in these brain regions compared to controls.
These findings indicate that older women who have experienced TBI exhibit greater vulnerability to long-term brain volume loss, especially in regions critical for memory and executive function.
Mechanistic Insights and Biological Plausibility
The observed sex differences may stem from several biological mechanisms. Hormonal influences, such as estrogen’s neuroprotective effects, could modulate brain resilience after injury and change with aging and menopause. Additionally, sex-specific inflammatory responses and genetic factors like APOE ε4 may differentially impact neurodegeneration post-TBI.
Hippocampal atrophy is a hallmark of neurodegenerative processes and is linked to impaired memory and increased risk of dementia. The frontal cortex governs executive functions, which are frequently compromised after brain injury. The preferential vulnerability of these brain regions in women highlights the need to explore sex-tailored neuroprotective strategies.
Controversies and Limitations
This study’s strengths include a well-characterized, community-based cohort with MRI imaging and detailed adjustment for confounders. However, limitations include the retrospective ascertainment of TBI history and potential recall bias. The majority of TBIs were mild, which may limit extrapolation to more severe injuries.
The time interval between injury and imaging was long but variable, and the study design cannot establish causality. Additionally, the underlying pathophysiological mechanisms remain to be clarified through longitudinal and experimental studies.
Conclusion
This research adds compelling evidence that traumatic brain injury has long-lasting, sex-specific effects on brain structure in older adults, with women showing greater brain volume loss in critical cognitive regions. These findings have important implications for risk stratification, monitoring, and therapeutic interventions following TBI, especially in women.
Further studies are warranted to elucidate the mechanisms underlying these sex differences and to develop targeted strategies that address the unique needs of women who have experienced brain injury.
References
Alzheimer’s Association International Conference (AAIC) 2025 Abstracts.
Gardner RC, et al. Sex differences in traumatic brain injury: A review. Neuropsychol Rev. 2018;28(4):408-419.
Bigler ED. Neuroimaging biomarkers in mild traumatic brain injury (mTBI). Neuropsychol Rev. 2013;23(3):169-209.
Whitney G, et al. Hormonal modulation of neuroinflammation and neuroprotection after traumatic brain injury: A review. J Neurotrauma. 2021;38(8):1076-1090.
Benedictus MR, et al. Hippocampal volume and cognitive decline: A systematic review. Neurology. 2015;85(19):1697-1704.