Highlights
- The FDA has approved SetPoint Medical’s vagus nerve stimulation (VNS) device for moderate-to-severe rheumatoid arthritis (RA) in patients failing or intolerant to biologic or targeted synthetic DMARDs.
- This is the first neuromodulatory device of its kind for RA, representing a new therapeutic class for refractory cases.
- Approval was based on a double-blind, sham-controlled trial (n=242) showing statistically significant improvement in ACR20 response rates and reduced DMARD dependency at one year.
- The device’s mechanism leverages the anti-inflammatory properties of the vagus nerve, opening new avenues for immunomodulation in systemic autoimmune disease.
Clinical Background and Disease Burden
Rheumatoid arthritis is a chronic, systemic autoimmune disease characterized by persistent synovitis, joint destruction, and systemic inflammation. Despite advances in therapy—including conventional, biologic, and targeted synthetic disease-modifying antirheumatic drugs (DMARDs)—a substantial proportion of patients remain refractory or intolerant to existing treatments. Such patients face ongoing pain, disability, and increased risk of comorbidities. The unmet need for safe and effective non-pharmacologic options remains high, especially in those who have exhausted available DMARDs or experienced unacceptable side effects.
Research Methodology
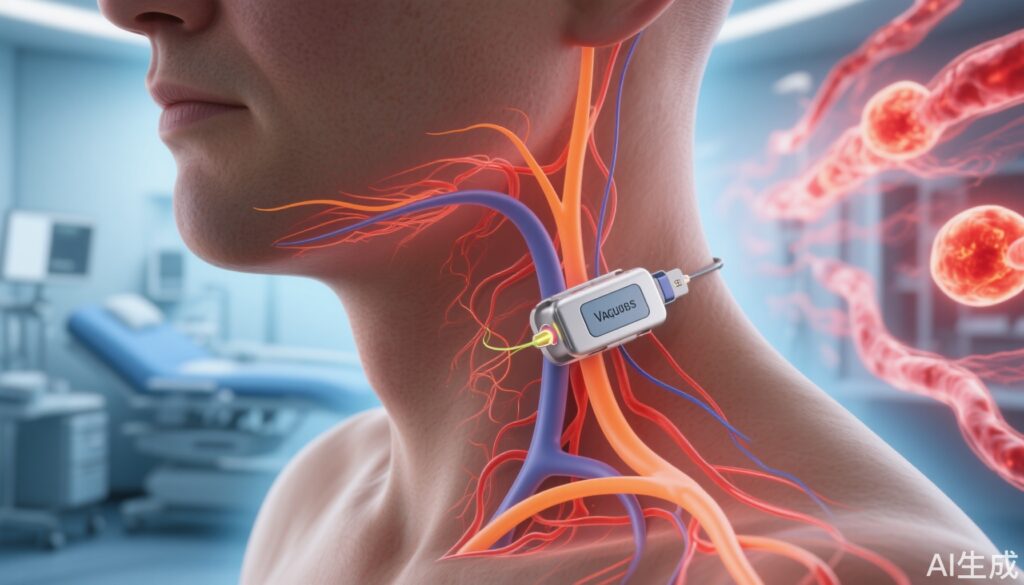
The approval of the SetPoint System was grounded in a randomized, double-blind, sham-controlled trial involving 242 patients with moderate-to-severe RA who had failed or could not tolerate biologic or targeted synthetic DMARDs. Patients were randomly assigned to receive either active VNS or a sham procedure. The device, roughly the size of a multivitamin, was implanted into the left cervical region and programmed to deliver one minute of vagus nerve stimulation daily. The primary endpoint was the proportion of patients achieving a ≥20% improvement in American College of Rheumatology response criteria (ACR20) at three months. Secondary endpoints included additional ACR response rates, changes in disease activity scores, and DMARD discontinuation rates over 12 months.
Key Findings
At three months, 35.2% of the active VNS group achieved ACR20 compared to 24.2% in the sham group—an absolute difference of 11 percentage points. While the magnitude of response is modest compared to some pharmacologic agents, statistical significance was achieved. Over 12 months, improvements in ACR response rates and disease activity metrics continued to accrue. Notably, at one year, 75% of trial participants were free from biologic or targeted synthetic DMARDs, suggesting that VNS therapy enabled significant drug tapering or discontinuation in a difficult-to-treat cohort. Adverse events related to device implantation were reported but were generally mild or moderate, consistent with other implantable neuromodulation devices.
| Endpoint | Active VNS | Sham | Absolute Difference |
|---|---|---|---|
| ACR20 at 3 Months | 35.2% | 24.2% | +11% |
| Free of Biologic/tsDMARDs at 1 Year | 75% | Data not reported | — |
Mechanistic Insights and Biological Plausibility
The vagus nerve plays a pivotal role in the inflammatory reflex, modulating immune responses through the cholinergic anti-inflammatory pathway. Preclinical and early-phase clinical studies have shown that electrical stimulation of the vagus nerve can suppress pro-inflammatory cytokine production, including TNF-α and IL-6, both central to RA pathogenesis. By targeting this neural-immune interface, the SetPoint System offers a non-pharmacologic immunomodulatory strategy distinct from current therapies.
Expert Commentary
Dr. John Tesser, a principal investigator in the pivotal trial, emphasized the clinical significance: “For patients with refractory RA who cannot tolerate or do not respond to biologics, this device offers a new avenue of hope. The ability to reduce or eliminate DMARD use in three-quarters of patients at one year is particularly promising.” Current guidelines from the American College of Rheumatology recommend escalation through DMARD classes; this device may now represent an option for those at the end of such algorithms.
Controversies and Limitations
While the trial results are promising, several limitations merit consideration. The absolute response rate, while statistically significant, may be viewed as modest, especially compared to newer biologic agents. The trial population was restricted to patients with moderate-to-severe disease, and generalizability to broader RA populations is unknown. Device implantation carries inherent surgical risks. Long-term durability, cost-effectiveness, and real-world adherence also require further study. Additionally, while adverse events were limited, the safety profile over several years remains undetermined.
Case Vignette
Consider Ms. Linda Thompson, a 54-year-old woman with seropositive RA who has failed methotrexate, etanercept, and tofacitinib due to inefficacy and intolerance. Facing persistent joint pain and elevated inflammatory markers, she undergoes SetPoint System implantation. Over 12 months, she experiences improvement in joint swelling and reports a reduction in pain medication use, allowing her to discontinue biologic therapy under her rheumatologist’s supervision.
Conclusion
The FDA approval of the SetPoint System marks a significant milestone in RA management, introducing neuromodulation as a new pillar for patients refractory to traditional and targeted DMARDs. While the device’s efficacy appears moderate, its ability to reduce DMARD dependency and its novel mechanism of action expand therapeutic possibilities for a difficult-to-treat patient subset. Continued surveillance and longer-term studies will be essential to define the device’s optimal place in therapy, safety profile, and cost-effectiveness.
References
1. Koopman FA, et al. Vagus nerve stimulation inhibits cytokine production and attenuates disease severity in rheumatoid arthritis. Proc Natl Acad Sci U S A. 2016;113(29):8284-8289.
2. Smolen JS, et al. Rheumatoid arthritis. Nat Rev Dis Primers. 2018;4:18001.
3. American College of Rheumatology. 2021 Guideline for the Treatment of Rheumatoid Arthritis. Arthritis Care Res (Hoboken). 2021;73(7):924-939.
4. SetPoint Medical. Press Release, July 31, 2024. [Accessed August 2024].
5. Presentation: 2024 American College of Rheumatology Annual Meeting, Washington, DC.