Study Background and Disease Burden
Chronic obstructive pulmonary disease (COPD) is a prevalent and progressive respiratory condition characterized by airflow limitation and chronic inflammation. It represents a leading cause of morbidity and mortality worldwide. A significant proportion of patients with COPD—estimated between 20% and 40%—exhibit an eosinophilic inflammatory phenotype, marked by elevated peripheral blood eosinophil counts. This subgroup tends to experience more frequent and severe exacerbations, which contribute substantially to the disease burden, impaired quality of life, and increased healthcare utilization.
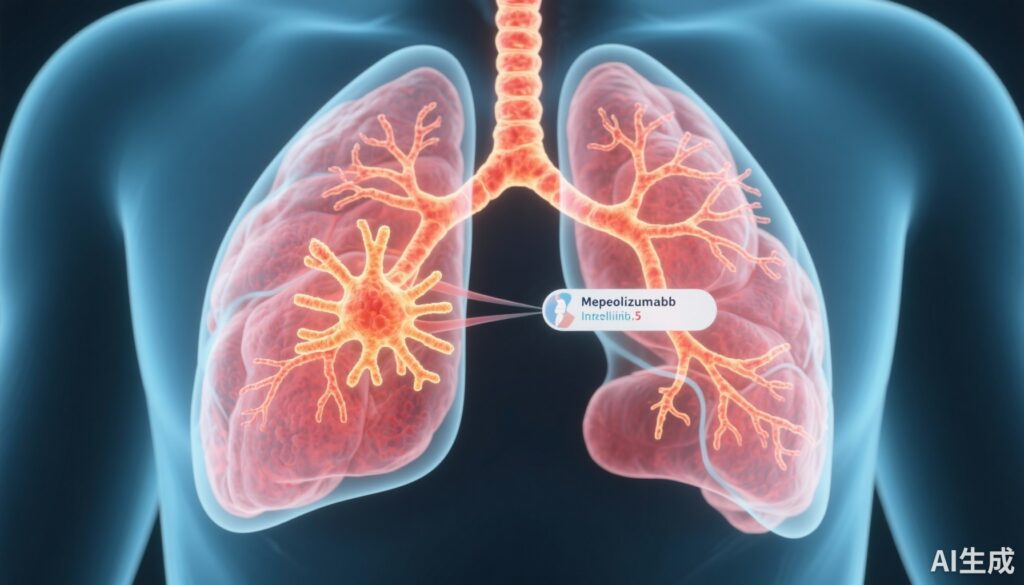
The pathophysiology of eosinophilic COPD involves eosinophil-driven inflammation, mediated largely by interleukin (IL)-5—a key cytokine responsible for eosinophil differentiation, recruitment, and survival. Traditional therapies including inhaled corticosteroids (ICS), long-acting beta-agonists (LABA), and long-acting muscarinic antagonists (LAMA) provide baseline control, but exacerbations persist in this high-risk cohort.
Mepolizumab, a humanized monoclonal antibody targeting IL-5, has shown clinical benefits in eosinophilic asthma by reducing exacerbations through eosinophil depletion. Its potential application in eosinophilic COPD addresses an unmet therapeutic need for targeted biologic treatment to reduce exacerbation frequency beyond standard inhaled therapies.
Study Design
The MATINEE trial was a phase 3, double-blind, randomized, placebo-controlled study designed to evaluate the efficacy and safety of mepolizumab in preventing exacerbations in COPD patients with an eosinophilic phenotype despite receiving optimized triple inhaled therapy. Eligible participants had a history of one or more moderate or severe exacerbations in the preceding year and a baseline blood eosinophil count ≥300 cells/µL.
A total of 804 patients were randomized 1:1 to receive either subcutaneous mepolizumab 100 mg or placebo every 4 weeks for a duration ranging from 52 to 104 weeks. The primary endpoint was the annualized rate of moderate or severe COPD exacerbations, with secondary hierarchical endpoints including time to first exacerbation, patient-reported outcomes related to health-related quality of life and symptoms, and exacerbations necessitating emergency department visits or hospitalizations. Multiplicity was controlled by testing secondary endpoints sequentially.
Key Findings
Among the 804 randomized patients, 403 received mepolizumab and 401 received placebo. Mepolizumab treatment resulted in a statistically significant 21% reduction in the annualized rate of moderate or severe COPD exacerbations compared with placebo (0.80 vs. 1.01 events per year; rate ratio 0.79; 95% CI, 0.66 to 0.94; P = 0.01).
The median time to first moderate or severe exacerbation was extended by nearly 100 days in the mepolizumab group versus placebo (419 vs. 321 days), with a hazard ratio of 0.77 (95% CI, 0.64 to 0.93; P = 0.009), indicating a delayed exacerbation onset.
Despite these encouraging reductions in exacerbation rates, no significant differences were observed between groups in patient-reported health-related quality of life or symptom measures. Because these endpoints were evaluated within a hierarchical testing framework, the lack of significance precluded formal statistical inference for subsequent secondary endpoints such as exacerbations leading to emergency department visits or hospitalizations.
The safety profiles of mepolizumab and placebo were comparable, with similar incidences of adverse events, supporting the tolerability of the intervention in this population on stable triple therapy.
Expert Commentary
The MATINEE trial provides robust evidence supporting the use of mepolizumab as an add-on therapy in COPD patients with an eosinophilic phenotype who continue to experience exacerbations despite maximal inhaled therapy. This aligns with emerging concepts underscoring the heterogeneity of COPD and the therapeutic potential of targeted biologics tailored to specific inflammatory endotypes.
However, the absence of improvement in patient-reported outcomes raises important considerations. It suggests that while mepolizumab effectively reduces exacerbation frequency, it may not directly translate into perceived symptomatic relief or quality of life enhancements within the study duration. The reasons may include multifactorial contributors to symptoms in COPD or the insensitivity of measured patient-reported instruments to capture changes related specifically to eosinophilic inflammation.
Furthermore, the trial’s stringent inclusion criteria—requiring elevated eosinophils and recent exacerbations despite triple therapy—define a high-risk subgroup wherein the benefits are most clearly demonstrable, but generalizability to broader COPD populations should be cautiously interpreted. Additional research might investigate long-term outcomes, effects on lung function decline, and cost-effectiveness analyses.
Conclusion
Mepolizumab significantly reduces the rate of moderate and severe COPD exacerbations when administered as an adjunct to triple inhaled therapy in patients with a confirmed eosinophilic phenotype. This represents a meaningful advancement in personalized COPD management, offering a targeted therapeutic option for a subgroup with considerable unmet needs. Nonetheless, the lack of detectable impact on quality of life metrics merits further investigation. Integration of mepolizumab into clinical practice will depend on diagnostic identification of eosinophilic phenotypes and balancing clinical benefits against economic considerations.
References
1. Sciurba FC, Criner GJ, Christenson SA, et al. Mepolizumab to Prevent Exacerbations of COPD with an Eosinophilic Phenotype. N Engl J Med. 2025 May 1;392(17):1710-1720. doi: 10.1056/NEJMoa2413181. PMID: 40305712.
2. Bafadhel M, Pavord ID, Russell REK. Eosinophils in COPD: Just another biomarker? Lancet Respir Med. 2017;5(9):747-759.
3. Vogelmeier CF, Criner GJ, Martinez FJ, et al. Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2024 Report: Global Strategy for Prevention, Diagnosis and Management of COPD. Am J Respir Crit Care Med. 2024;209(9):1231-1245.