Highlight
- Delayed hyponatremia is a leading cause of readmission after endoscopic endonasal transsphenoidal surgery (EETS) for pituitary neuroendocrine tumors (PitNET).
- Postoperative fluid restriction (FR) from postoperative day (POD) 3 to 14 reduces the incidence and severity of delayed hyponatremia.
- Strict fluid restriction (1–1.2 L/day) significantly lowered severe hyponatremia rates to zero and decreased hospital readmission compared to ad-lib fluid intake.
- Further investigations are warranted to define the optimal volume and timing for fluid restriction after EETS.
Study Background and Disease Burden
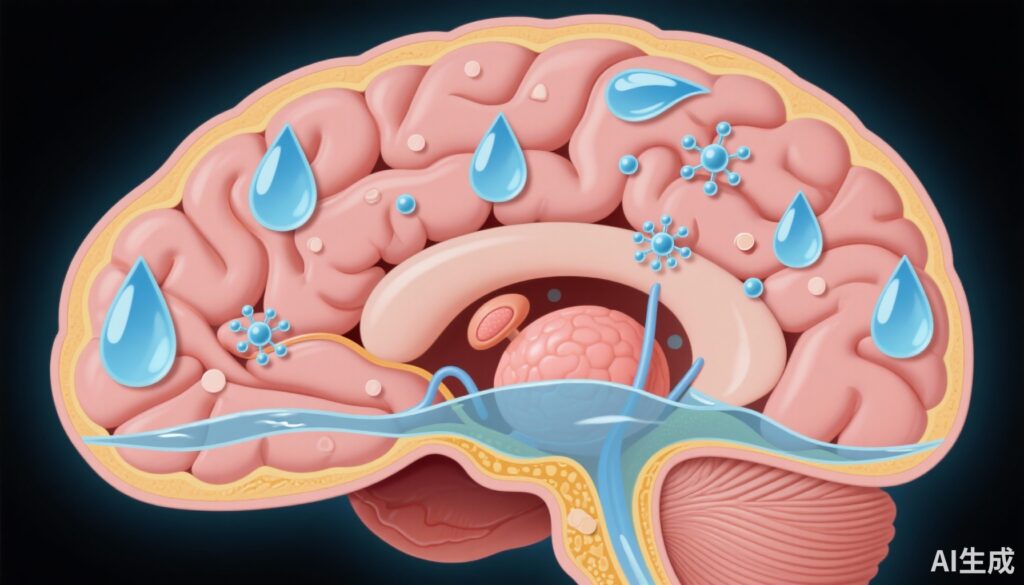
Endoscopic endonasal transsphenoidal surgery (EETS) is a common surgical approach for removing pituitary neuroendocrine tumors (PitNETs) and other sellar region pathologies. Despite being minimally invasive, this procedure carries postoperative risks, notably delayed hyponatremia, a disturbance in serum sodium levels typically occurring after hospital discharge. Delayed hyponatremia can induce significant clinical symptoms ranging from nausea, headache, and lethargy to severe neurological complications including seizures and coma, often necessitating hospital readmission. This postoperative electrolyte imbalance arises from disrupted water and sodium homeostasis, commonly related to inappropriate antidiuretic hormone secretion.
Given the substantial morbidity and healthcare burden associated with readmissions for hyponatremia following EETS, effective preventative strategies are critically needed. Previous observational studies have suggested that postoperative fluid restriction might mitigate this risk by reducing free water intake and limiting dilutional hyponatremia. However, there was insufficient high-quality prospective evidence to define optimal fluid restriction protocols or their efficacy in preventing delayed hyponatremia.
Study Design
This prospective randomized controlled trial enrolled 300 patients scheduled for EETS between 2016 and 2023 at a single institution. Exclusion criteria encompassed patients with chronic kidney disease, congestive heart failure, arginine vasopressin deficiency detected by postoperative day (POD) 3, chronic hyponatremia, or untreated adrenal insufficiency or hypothyroidism, to minimize confounding conditions affecting sodium balance.
Participants were randomized postoperatively into three groups: a control group allowed ad libitum fluid intake (n = 94), a moderate fluid restriction (FR) group receiving 1.8 L/day (or 2 L/day for patients >100 kg; n = 39), and a strict FR group limited to 1 L/day (or 1.2 L/day for patients >100 kg; n = 62). Fluid restriction was implemented from POD 3 through POD 14, the critical window during which delayed hyponatremia most commonly occurs.
The primary endpoints included the incidence of overall hyponatremia (serum sodium <135 mEq/L), moderate hyponatremia (serum sodium 125-129 mEq/L), and severe hyponatremia (serum sodium <125 mEq/L). Secondary outcomes comprised hospital readmission rates, daily fluid intake measurements, and patient-reported thirst levels, assessing tolerability of interventions.
Key Findings
The study revealed a stepwise reduction in hyponatremia incidence with increasing fluid restriction severity. Overall hyponatremia rates were 31.9% in the control group, 28.2% in the moderate FR group, and 21.0% in the strict FR group. Importantly, severe hyponatremia occurred in 7.4% of controls, 5.1% in the moderate FR group, and was completely eliminated (0%) in the strict FR group.
Statistical analysis confirmed the strict FR cohort had a significantly higher nadir serum sodium level by an average of 1.81 mEq/L compared to controls (95% CI: 0.34 to 3.27; P = .02) and a significantly lower incidence of severe hyponatremia (95% CI, 0.00 to 1.02; P = .04). Hospital readmission rates reflected these biochemical improvements, with 6.4% readmission in the control arm versus 1.6% in the strict FR arm.
In assessing tolerability, although strict FR necessitated greater limitation of oral fluids, patients did not report clinically concerning increases in thirst, suggesting that strict fluid restriction from POD 3 to 14 is feasible in a postoperative setting.
Expert Commentary
This study meaningfully advances our understanding of postoperative management after EETS by rigorously evaluating fluid restriction as a preventative measure against delayed hyponatremia. The randomized controlled design and exclusion of confounding comorbidities strengthen the validity and generalizability of the findings within this surgical population.
The complete elimination of severe hyponatremia in the strict FR group is remarkable and suggests a compelling protective effect. However, the moderate FR group had only a modest reduction, indicating that fluid restriction below a critical volume threshold may be necessary to yield significant clinical benefit.
Current consensus guidelines on the prevention of postoperative hyponatremia after pituitary surgery remain vague regarding fluid management, often relying on institutional protocols or expert opinion. This trial provides empirical data supporting postoperative fluid restriction to reduce a common and dangerous complication.
Limitations include its single-center scope and relatively small sample size in the FR arms, which may affect power to detect smaller differences or adverse events. Furthermore, the study did not stratify outcomes by specific tumor types or hormonal statuses, which could influence sodium regulation.
Mechanistically, fluid restriction likely limits free water excess that exacerbates dilutional hyponatremia, particularly during the syndrome of inappropriate antidiuretic hormone secretion (SIADH) phase observed after pituitary surgery. Thus, carefully titrated FR may restore a favorable osmotic balance and prevent symptomatic sodium declines.
Conclusion
Postoperative fluid restriction from POD 3 to 14 significantly reduces delayed hyponatremia incidence, eliminates severe hyponatremia, and decreases hospital readmission after endoscopic endonasal transsphenoidal surgery for PitNET and sellar pathology. Strict fluid restriction to approximately 1 to 1.2 liters daily was most effective and well tolerated.
These findings support implementing postoperative fluid restriction as a standard care component to improve outcomes and reduce complications in this population. Further multicenter studies with larger sample sizes are needed to refine optimal fluid volumes, duration, and patient selection criteria to maximize efficacy and safety.
References
1. Klaassen D, Mok S, Hwang JY, Blount SL, Williams KJ, Fong BM, et al. Postoperative fluid restriction to prevent delayed hyponatremia after endoscopic transsphenoidal surgery. Neuro Oncol. 2025 Sep 8;27(7):1746-1757. doi: 10.1093/neuonc/noaf069. PMID: 40084913; PMCID: PMC12417837.
2. Sherlock M, O’Sullivan EP, Agha A, Tormey W, Behan LA, Owens D, et al. Hyponatraemia in patients after pituitary surgery: syndrome of inappropriate antidiuretic hormone secretion or cerebral salt wasting? Clin Endocrinol (Oxf). 2009 Oct;71(4):481-5. doi: 10.1111/j.1365-2265.2008.03404.x.