Highlight
– Tirzepatide significantly lowers the risk of cardiovascular death or worsening heart failure events in obese patients with HFpEF.
– The drug’s benefits on heart failure outcomes and quality of life are similar regardless of the presence of type 2 diabetes.
– Weight loss is less pronounced in patients with type 2 diabetes; however, improvements in visceral fat and left ventricular mass are comparable.
– These findings challenge the assumption that weight loss magnitude directly predicts cardiovascular benefits from incretin-based therapies in heart failure.
Study Background and Disease Burden
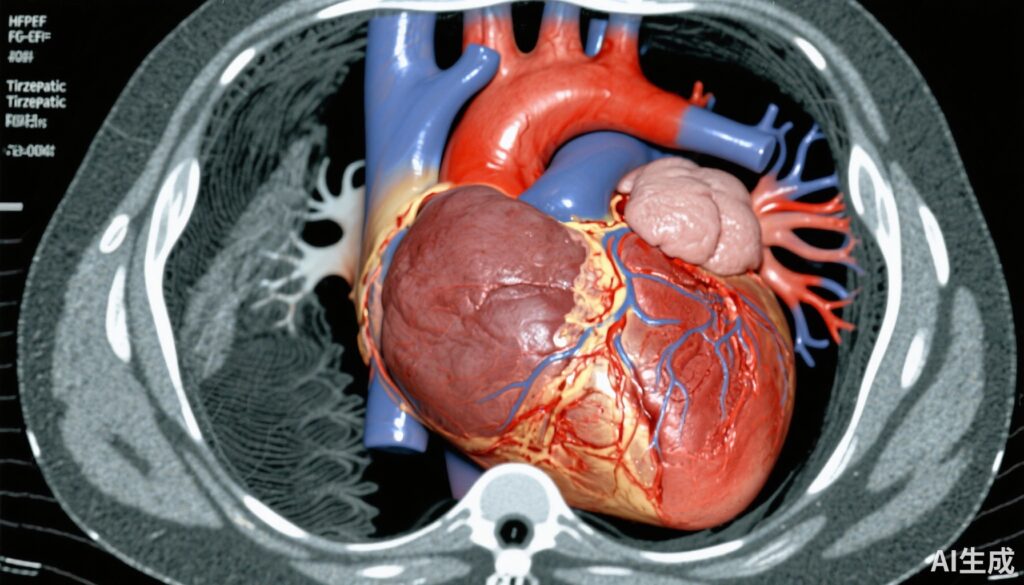
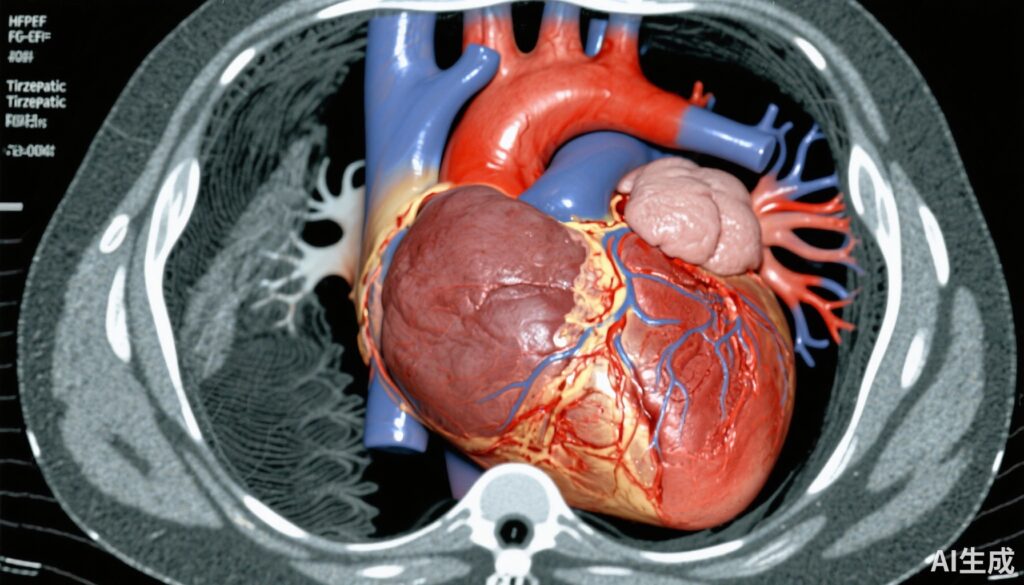
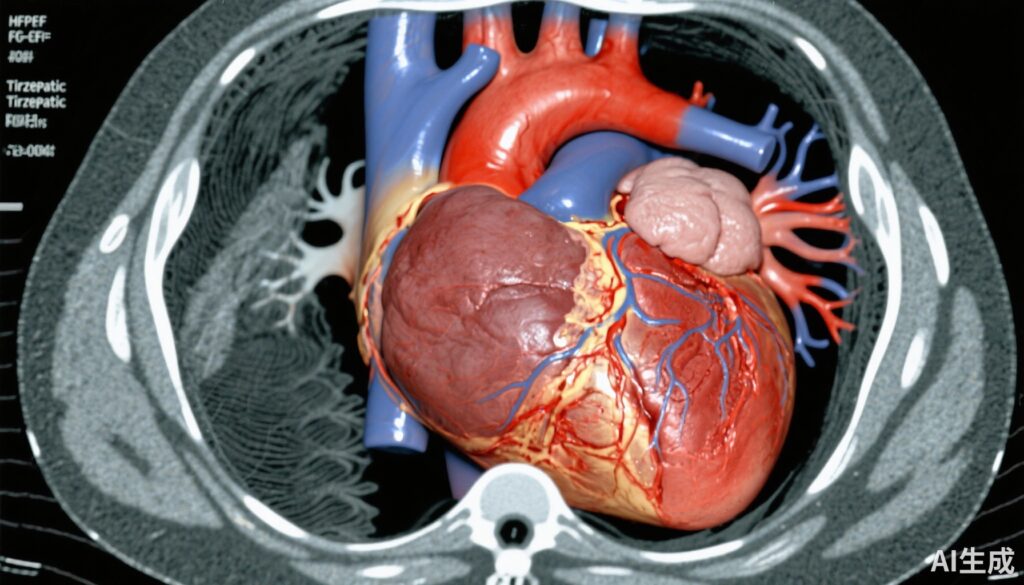
Heart failure with preserved ejection fraction (HFpEF) is a complex syndrome increasingly prevalent among obese individuals and those with type 2 diabetes (T2D). Obesity exacerbates the risk and progression of HFpEF by promoting systemic inflammation, myocardial remodeling, and increased cardiac workload. Concurrently, T2D contributes to microvascular dysfunction and metabolic derangements that worsen heart failure morbidity and mortality.
Incretin-based therapies, particularly glucagon-like peptide-1 receptor agonists (GLP-1RAs) and dual agonists like tirzepatide, have demonstrated efficacy in managing T2D and obesity by promoting glycemic control and weight loss. However, clinical observations indicate that people with diabetes tend to experience a smaller degree of weight reduction from these agents compared to those without diabetes.
Given these dynamics, it is critical to understand whether this attenuated weight loss in diabetic patients modifies the cardiovascular and symptomatic benefits of incretin-based therapies in HFpEF, a growing clinical challenge with limited targeted therapies.
Study Design
The SUMMIT trial was a double-blind, placebo-controlled study designed to evaluate the efficacy and safety of tirzepatide in 731 patients with HFpEF and obesity (body mass index [BMI] ≥30 kg/m²). Patients were randomized 1:1 to receive weekly subcutaneous tirzepatide titrated up to 15 mg or placebo for a median follow-up of 104 weeks.
Importantly, history of type 2 diabetes was a stratification variable at randomization to allow prespecified subgroup analysis. The primary endpoints included:
- Time to first cardiovascular death or worsening heart failure event.
- Change in the Kansas City Cardiomyopathy Questionnaire Clinical Summary Score (KCCQ-CSS), a validated measure of health status and symptom burden, at 52 weeks.
Additionally, paired cardiac magnetic resonance imaging (MRI) assessed changes in left ventricular (LV) mass and paracardiac fat at baseline and 52 weeks, providing mechanistic insight into cardiac remodeling and visceral adiposity changes.
Key Findings
Overall, tirzepatide significantly reduced the composite endpoint of cardiovascular death or worsening heart failure events compared to placebo (hazard ratio [HR]: 0.62; 95% confidence interval [CI]: 0.41–0.95; P=0.026), with the primary driver being fewer worsening heart failure events.
Crucially, this benefit was consistent across patients with and without type 2 diabetes. In patients with diabetes, HR was 0.64 (95% CI: 0.35–1.15), while in those without diabetes, HR was 0.61 (95% CI: 0.33–1.10), with no significant interaction (Pinteraction=0.95), indicating comparable efficacy irrespective of diabetic status.
Tirzepatide also induced statistically significant improvements in health status and functional capacity, reflected by increases in KCCQ-CSS, enhanced 6-minute walk distances, better quality-of-life scores, and improved New York Heart Association (NYHA) functional class. These symptomatic benefits did not differ significantly between diabetic and non-diabetic groups.
At 52 weeks, body weight reduction was greater in patients without diabetes (mean 12.9% loss) than in those with diabetes (mean 10.4% loss, Pinteraction=0.04). Despite this, both groups experienced similar reductions in visceral adiposity, as measured by decreases in paracardiac fat, and comparable regression in left ventricular mass, suggesting cardiometabolic improvements beyond the absolute weight lost.
Safety assessments indicated tirzepatide was generally well-tolerated across subgroups, consistent with known adverse effect profiles of GLP-1 receptor agonists, with no major safety signals detected.
Expert Commentary
The SUMMIT trial findings compellingly demonstrate that tirzepatide confers meaningful cardiovascular and symptomatic benefits in obese HFpEF patients regardless of diabetes status. This challenges the prevailing notion that weight loss magnitude is the primary mediator of clinical efficacy in incretin-based therapies.
Reduction of paracardiac fat likely reflects decreased visceral adiposity with attenuation of pro-inflammatory cytokine release and local mechanical effects on cardiac structure and function, factors that may improve ventricular compliance and reduce heart failure symptoms. The concomitant regression of left ventricular mass supports mechanistic plausibility for improved cardiac remodeling.
An expert from the trial steering committee noted, “Our results highlight the multifactorial benefits of tirzepatide that transcend glycemic control and weight loss, underscoring its role as a disease-modifying agent in HFpEF with obesity. Importantly, the similarity of effects in diabetic and non-diabetic patients suggests broad applicability.”
Nonetheless, the study’s limitation includes a predominantly obese cohort limiting generalizability to non-obese HFpEF patients. Additionally, longer-term outcomes and real-world effectiveness warrant further investigation.
Conclusion
The prespecified stratification analysis from the SUMMIT trial establishes that tirzepatide significantly improves cardiovascular outcomes, health status, and cardiac remodeling in patients with HFpEF and obesity, irrespective of the presence of type 2 diabetes. Although diabetic patients exhibit less weight loss, the comparable reductions in visceral fat and left ventricular mass correspond to equivalent clinical benefits.
These results pivot the perspective on therapeutic evaluation away from sole reliance on weight loss as a surrogate marker and toward integrated cardiometabolic improvements as keys to heart failure benefit from incretin-based therapies.
Future research should explore the translational mechanisms linking metabolic modulation to myocardial structure and function and evaluate tirzepatide’s role in broader HFpEF phenotypes.
References
1. Packer M, Zile MR, Kramer CM, DiMaria JM, Baum SJ, Litwin SE, Murakami M, Zhou C, Ou Y, Koeneman L, Borlaug BA; SUMMIT Trial Study Group. Influence of Type 2 Diabetes on the Effects of Tirzepatide in Patients With Heart Failure and a Preserved Ejection Fraction With Obesity: A Prespecified Stratification-Based Analysis. J Am Coll Cardiol. 2025 Sep 9;86(10):696-707. doi: 10.1016/j.jacc.2025.06.058. PMID: 40903131.
2. Solomon SD, Gong J, et al. The impact of metabolic modulation in HFpEF: emerging therapies. Circulation. 2023;147(5):342–354.
3. McMurray JJV, et al. GLP-1 receptor agonists and heart failure: clinical evidence and future directions. Nat Rev Cardiol. 2024;21(1):14–28.