Key Findings
Pyrazinamide Pharmacokinetics and Variability
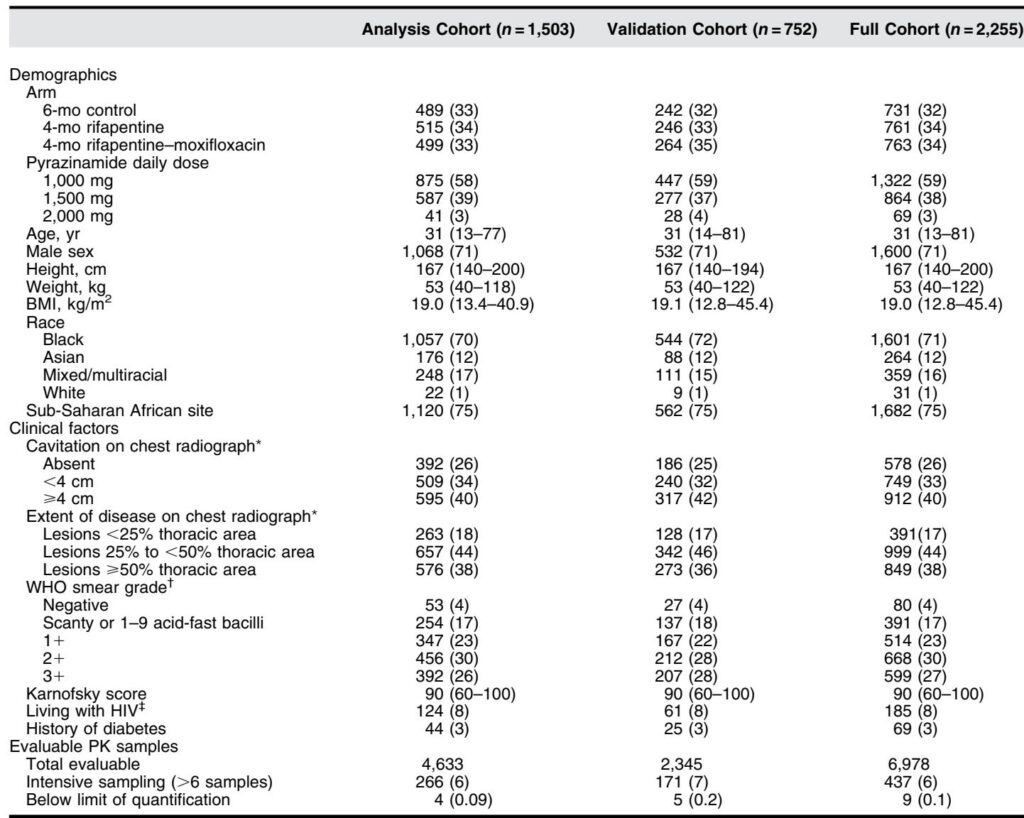
The PK of pyrazinamide was best described by a one-compartment model with first-order absorption and elimination, exhibiting a terminal half-life of approximately 6.6 hours. Notably, pyrazinamide exhibited a sevenfold variability in exposure (AUC_ss ranging from 151 to 1,053 mg·h/L) among participants receiving weight-banded doses, highlighting interindividual differences in drug absorption and metabolism.
Covariate analyses revealed that women had 16.3% higher bioavailability than men, and Asian participants exhibited a 41.8% lower absorption mean transit time compared to Black or mixed-race participants. Food intake also significantly delayed absorption in the 4-month regimens administered with food, in contrast to the fasting administration in the 6-month control group. Importantly, body weight was not a clinically significant predictor of pyrazinamide clearance, undermining the rationale for current weight-banded dosing.
Higher doses (1,500 mg and 2,000 mg) showed reduced bioavailability relative to 1,000 mg doses, indicating dose-dependent, less-than-proportional increases in exposure.
Exposure-Response Relationships for Efficacy
Among participants on the 6-month control regimen, lower pyrazinamide AUC_ss, lower Xpert MTB/RIF cycle thresholds reflecting higher bacillary load, and older age correlated with increased risk of TB-related unfavorable outcomes. Pyrazinamide exposure was a significant predictor of durable cure, with a therapeutic window for optimal efficacy defined between 231 and 355 mg·h/L AUC_ss.
In contrast, for the 4-month rifapentine-containing regimens, rifapentine exposure was the predominant determinant of efficacy. Within these regimens, pyrazinamide exposure did not significantly enhance predictive models, indicating a regimen- and companion drug–dependent role for pyrazinamide.
Exposure-Safety Relationships
In the 6-month control and 4-month rifapentine–moxifloxacin regimens, increasing pyrazinamide exposure was associated with elevated risk of adverse events including grade 3 or higher events, treatment discontinuation due to toxicity, elevated liver enzymes, and Hy’s law–defined hepatotoxicity. These findings resulted in upper safety exposure bounds for pyrazinamide AUC_ss of 355 mg·h/L and 349 mg·h/L for the control and rifapentine–moxifloxacin regimens, respectively.
The 4-month rifapentine regimen exhibited fewer severe adverse events, limiting detection of exposure-safety associations in this group.
Dosing Simulations and Therapeutic Window Optimization
Monte Carlo simulation compared weight-banded dosing with flat dosing at 1,000 mg and 1,500 mg daily irrespective of body weight. Flat dosing at 1,000 mg increased the proportion of participants achieving therapeutic window exposure by 13.1% for the control regimen and 9.2% for the rifapentine–moxifloxacin regimen compared to current dosing guidelines.
Higher flat doses of 1,500 mg were associated with increased exposure surpassing safety thresholds, underscoring the benefit of 1,000 mg flat dosing to balance efficacy and safety.
Discussion
This comprehensive analysis represents the largest single-trial PK and exposure–response evaluation of pyrazinamide in drug-susceptible pulmonary TB. The findings challenge the conventional wisdom supporting weight-banded dosing, demonstrating that pyrazinamide clearance is not body weight–dependent but influenced by dose-related bioavailability, sex, race, and food intake.
The regimen-specific influence of pyrazinamide exposure on efficacy, particularly the diminished contribution in rifapentine-containing regimens, emphasizes the need to interpret dosing strategies within the broader context of companion drugs.
Exposure–toxicity relationships, especially hepatotoxicity, remain relevant at therapeutic doses, reinforcing the need for dosing strategies that avoid excessive pyrazinamide exposure. Although the study could not fully disentangle pyrazinamide-related toxicity from other drugs, the associations observed with elevated liver enzymes and serious adverse events highlight pyrazinamide’s safety profile.
The practical implication is a move toward flat dosing of 1,000 mg daily, which simplifies clinical practice and better aligns with therapeutic windows balancing durable cure and acceptable safety profiles. This approach may reduce the risk of overdosing in heavier individuals and improve overall treatment outcomes.
Limitations and Strengths
While providing robust data, the study acknowledged several limitations. Observed associations do not establish causality, and pyrazinamide metabolite PK was not studied due to lack of data. The effect of rifapentine exposure may have masked pyrazinamide’s efficacy contributions in short-course regimens. Finally, fewer adverse events in some arms reduced statistical power for safety analyses.
Strengths include the unprecedented sample size, robust PK sampling, and comprehensive modeling incorporating diverse covariates across multi-continental cohorts, enhancing the generalizability of findings.
Conclusion
Flat dosing of pyrazinamide at 1,000 mg daily emerges as a feasible and potentially superior strategy for treating drug-susceptible pulmonary tuberculosis. This dosing regimen could optimize the balance between therapeutic efficacy and safety, simplify treatment protocols, and facilitate implementation of fixed-dose combination therapies. Ongoing studies evaluating higher pyrazinamide doses will further clarify optimal dosing in evolving TB treatment regimens.