Background and Disease Burden
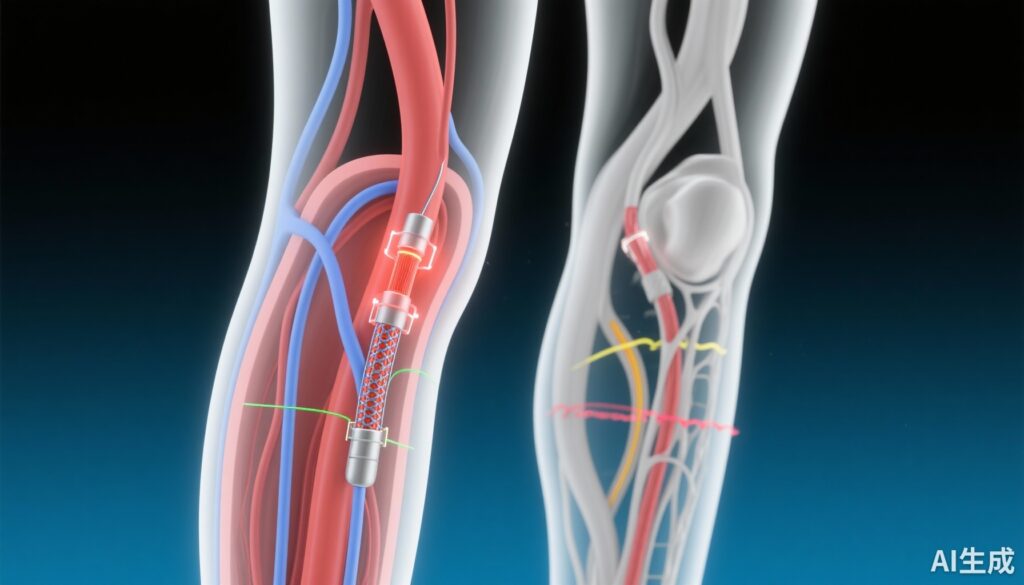
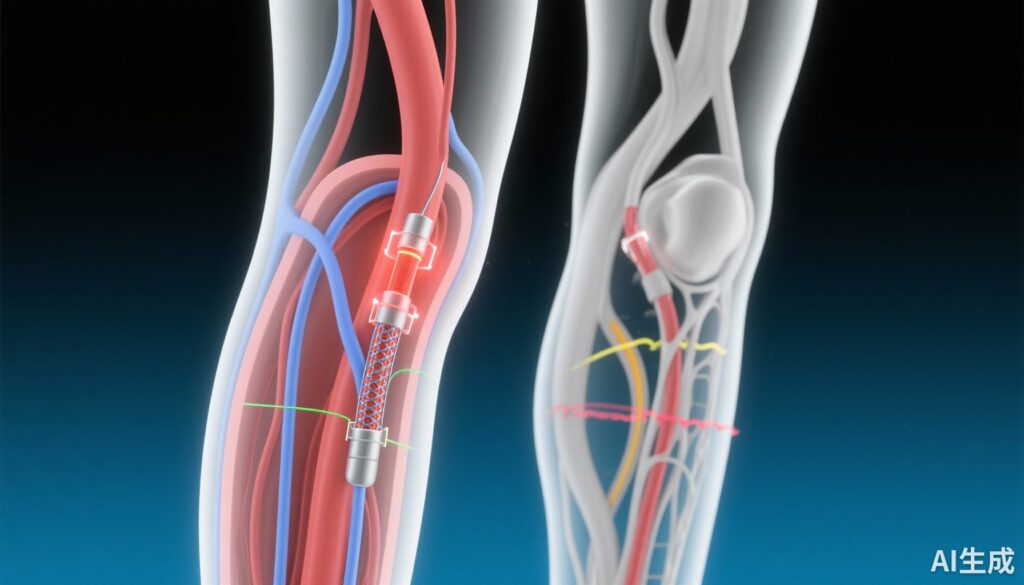
Chronic limb-threatening ischaemia (CLTI) is the most severe form of peripheral artery disease (PAD), characterized by critical reductions in limb perfusion, often manifested as rest pain, ulcers, or gangrene (Rutherford categories 4-6). CLTI affects millions globally and carries significant risks of limb loss and mortality. Infrainguinal endovascular revascularisation has emerged as a key therapeutic approach to restore blood flow and prevent amputations. Drug-coated devices, particularly paclitaxel-coated balloons and stents, were developed to reduce restenosis by inhibiting neointimal hyperplasia. While these devices are commonly used in coronary and peripheral interventions, their impact on hard clinical endpoints in CLTI, specifically above-ankle major amputation rates, remains uncertain. Previous meta-analyses and studies raised concerns about potential increased mortality associated with paclitaxel-coated devices, further complicating their clinical use. Thus, the SWEDEPAD 1 trial was designed to address the critical question of whether paclitaxel-coated devices improve limb salvage outcomes compared to uncoated devices in patients with advanced PAD undergoing infrainguinal endovascular treatment.
Study Design
The Swedish Drug-Elution Trial in Peripheral Arterial Disease 1 (SWEDEPAD 1) is a pragmatic, nationwide, multicentre, participant- and outcome-assessor masked, registry-based, randomised controlled trial. Conducted at 22 centres across Sweden, it enrolled adult patients with Rutherford category 4-6 PAD scheduled for infrainguinal revascularisation.
Eligibility required successful guidewire crossing of the target lesion. Participants were randomly allocated 1:1 after successful lesion crossing to either receive paclitaxel-coated balloons or stents or uncoated devices. Randomisation was computer-generated with stratification by centre, using a secure allocation concealed via an embedded web system in the Swedish vascular registry. This registry-based design enabled efficient follow-up and comprehensive outcome capture.
The primary efficacy endpoint was ipsilateral major amputation, defined as above-ankle amputation, during the follow-up period extending up to 5 years. Secondary endpoints included all-cause mortality and safety assessments. Analyses were performed on an intention-to-treat basis. The trial was prospectively registered (ClinicalTrials.gov NCT02051088).
Key Findings
Between November 2014 and September 2023, 2400 patients were randomized, with 1206 assigned to paclitaxel-coated devices and 1194 to uncoated devices. The intention-to-treat analysis included 2355 patients (1180 paclitaxel-coated, 1175 uncoated). Patients had a median age of 77 years, and 56% were male. Notably, over half (52.6%) had diabetes, a major risk factor for poor outcomes in PAD. The majority (74.9%) presented with tissue loss or wounds classified as Rutherford stage 5 or 6, reflecting a high-risk CLTI population.
Target lesions were predominantly located in the femoropopliteal segment (52.7%), with others in infrapopliteal arteries or both segments. Paclitaxel was the coating agent in >99% of drug-coated devices.
During a median follow-up of 2.67 years, the primary endpoint, ipsilateral major amputation, occurred at similar rates between groups. The hazard ratio (HR) for amputation with paclitaxel-coated devices relative to uncoated devices was 1.05 (95% confidence interval [CI] 0.87-1.27; p=0.61), indicating no statistically significant or clinically meaningful difference. All-cause mortality was also comparable, with an HR of 1.04 (95% CI 0.92-1.17; p=0.54).
These findings stand in contrast to earlier concerns from meta-analyses hinting at excess mortality with paclitaxel-coated devices, but support the devices’ safety with regard to limb salvage and survival in a real-world, advanced PAD population.
Expert Commentary
The SWEDEPAD 1 trial is notable for its large sample size, rigorous randomized design, and extended follow-up, addressing prior gaps in evidence regarding paclitaxel-coated devices in CLTI. Its pragmatic, registry-based methodology enhances generalizability and efficiency, capturing data from a real-world patient cohort with extensive comorbidities and advanced disease.
The lack of benefit in reducing major amputations suggests that the antiproliferative effects of paclitaxel may be insufficient on their own to overcome the complex pathophysiology of severe limb ischemia, including extensive microvascular disease common in diabetes. This challenges the assumption that drug-coated devices translate to improved hard clinical outcomes in this population, despite their clear efficacy in reducing restenosis rates in less advanced PAD.
Moreover, no safety signal emerged for mortality, reassuring clinicians but underscoring the necessity of careful patient selection and further research on device technology and adjunctive therapies.
Limitations include the absence of data on quality of life, functional outcomes, and detailed lesion characteristics such as calcification, which may influence response to intervention. Longer-term follow-up and subgroup analyses (e.g., by diabetes status or lesion location) will provide further insights.
Conclusion
The SWEDEPAD 1 trial provides robust evidence that paclitaxel-coated devices do not reduce ipsilateral major amputations nor affect all-cause mortality compared with uncoated devices in patients with chronic limb-threatening ischaemia undergoing infrainguinal endovascular revascularisation. While these devices remain valuable tools for reducing restenosis in PAD, their role in improving meaningful limb salvage in advanced disease is unproven.
Clinicians should weigh these findings in therapeutic decision-making and counsel patients accordingly. Future research should focus on novel drug coatings, combination therapies targeting microvascular disease, and personalized revascularisation strategies to improve outcomes in this challenging population.
References
Falkenberg M, James S, Andersson M, et al; SWEDEPAD trial investigators. Paclitaxel-coated versus uncoated devices for infrainguinal endovascular revascularisation in chronic limb-threatening ischaemia (SWEDEPAD 1): a multicentre, participant-masked, registry-based, randomised controlled trial. Lancet. 2025;406(10508):1103-1114. doi:10.1016/S0140-6736(25)01585-5
Norgren L, Hiatt WR, Dormandy JA, et al. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). Eur J Vasc Endovasc Surg. 2007;33 Suppl 1:S1-75.
Rocha-Singh KJ, Duval S, Jaff MR, et al. Mortality and Paclitaxel-Coated Devices: An Individual Patient Data Meta-Analysis. Circulation. 2020;141(19):1503-1515. doi:10.1161/CIRCULATIONAHA.120.047430
Farber A, Eberhardt RT. The Current State of Critical Limb Ischemia: A Systematic Review. JAMA Surg. 2016;151(11):1070-1077. doi:10.1001/jamasurg.2016.2314